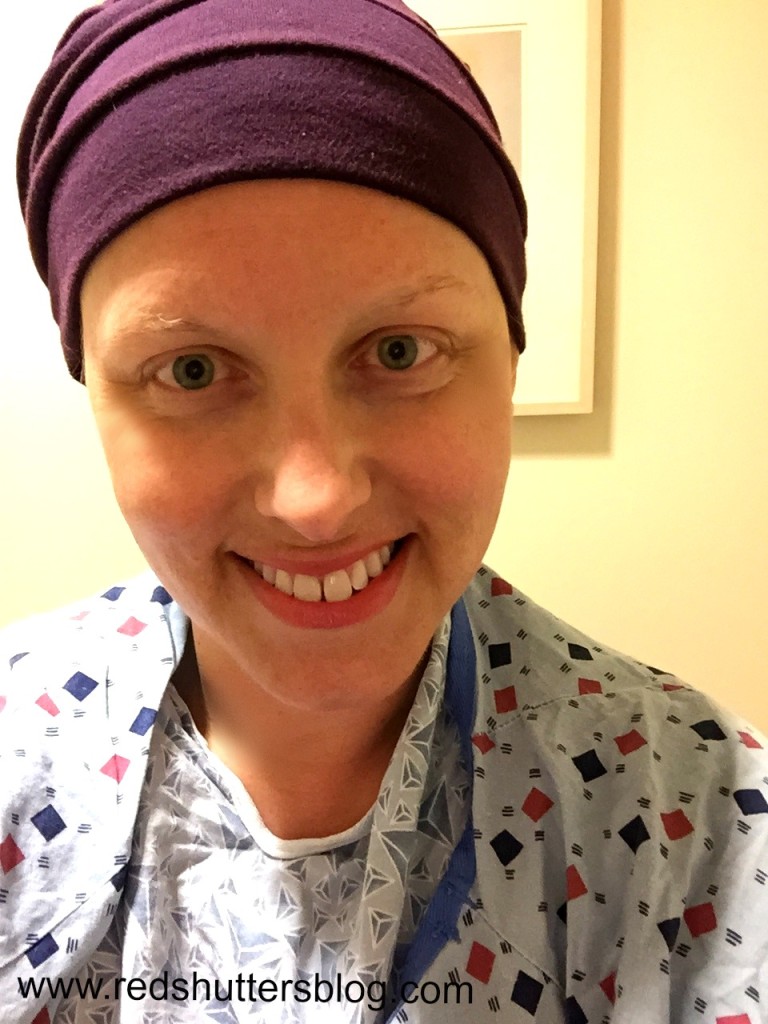
This photo is of me on my last day of breast cancer radiation therapy. That robe is the height of fashion, amiright?
“You’re doing great. I think we won’t torture you with anymore follow up visits. You’re all done with us. If you have questions, let me know, of course.”
My radiation oncologist had a big smile on her face, as she bid me farewell earlier this week. We said good-bye and extended to each other our best wishes. With those words, another phase of my breast cancer treatment—radiation therapy—was over.
I had radiation therapy this summer. My treatment lasted four weeks, with treatments on five days a week, Monday through Friday. After chemotherapy, which was my least favorite activity ever (and that includes childbirth), I thought radiation would be a breeze. A breeze, it was not.
Not every breast cancer patient needs radiation. Those who do have different lengths of treatment; my experience, therefore, isn’t exactly what everyone else goes through but it’s similar enough to give you a sense of what to expect.
The first thing I learned about radiation is that a doctor different from my primary oncologist was assigned to manage my care. Just as a surgeon oversaw my surgery, a radiation oncologist, working in conjunction with my primary oncologist, directed this part of my treatment.
While still undergoing chemotherapy, I met with my radiation oncologist for an initial consultation, bringing along a friend for moral support (I always recommend attending important medical appointments with someone else, as it’s so hard to hear and understand everything the doctor says). That meeting was helpful in explaining the details of radiation and alleviating my concerns. I jokingly asked if I would glow in the dark due to the radiation, and the doctor looked very concerned, misunderstanding that I was kidding. She was quick to assure me I wouldn’t, and explained that I wasn’t the only one to ask this question—though other people seriously thought they would glow in the dark or be radioactive. Apparently, it’s a misconception about radiation therapy.
For some, the purpose of radiation is to shrink a tumor. For me, the goal of radiation was to kill off any cancer cells that were still hanging around after surgery and chemotherapy. As a result, radiation is targeted, meaning that it is focused only on the site where cancer has been found. For me, the duration and target of radiation was determined in a second appointment, during which a number of measurements are taken. The radiation oncologist, working with a physicist and other members of the radiation therapy team, used the measurements to program the machine delivering the radiation and to figure out how long the therapy should last. At my consultation, I was told that radiation for people with my type of breast cancer would be, on average, between four and six weeks. After the measurements were calculated, my radiation therapy was determined to be four weeks, which was a relief; coming off of chemotherapy, I wanted to move through this next phase as quickly as possible.
The first radiation therapy appointment had me stressed, I’ll admit. It was the stress of a new experience; despite being prepared by my doctor and her team, I was still uncertain how it would all go. The radiation oncology team at Dana Farber works hard to make this process as easy as possible for patients, from having the most friendly people welcoming patients, to assigning special parking spots to radiation oncology patients, and to even covering the costs of parking—which is especially helpful when you are there five days a week for weeks on end.
What surprised me most about that first treatment, though, was how easy it was. I scanned in my radiation card at the front desk, which alerted the team that I had arrived. (I had been given the card on a previous visit.) I changed into a robe, leaving on my clothes from the waist down. Hats, scarves, and wigs were okay, too, which was helpful since most of the women I saw in the waiting room wore one of these during treatment. Snacks and reading material was plentiful, though the wait to be called into the treatment room was never long for me to enjoy the latest issue of People. Sometimes, I chatted with other women waiting for treatment, and I found that people were most talkative during their last week of radiation. There was something about being almost done that made people relax a bit, celebrating perhaps or just really breathing for the first time.
When it was my turn, I was called into the treatment room by one of the warm and encouraging technicians. I handed one of them my card, so they could scan me into the machine. I hopped up on the machine, lying down under the laser (it’s probably not really called a laser—that might be a bit too sci fi—but it’s what it looked like to me). The technicians confirmed the calculations specific to my treatment and lined me up under the machine, using my radiation tattoos as a guide. The tattoos—four small blue dots—had been placed on my chest during that appointment when my measurements were taken. They were the way the team targeted the radiation, making sure to direct it correctly (i.e., to where the cancer had been found and not at my heart and lungs). The technicians then left the room, speaking to me from the control room via an intercom system. They’d ask me to hold my breath, and they would begin the treatment, with a clicking sound signifying that the radiation was being “shot” at me. This repeated a few times, and then I was done. The entire process lasted about eight minutes and that’s not an exaggeration; I timed it. Sometimes, such as on Mondays when our greetings last longer as we recounted our weekend plans, it may have been a minute or two longer.
Only eight minutes. It took longer to drive to the hospital—one way!—than it took to deliver the radiation therapy.
Once a week, I met with my radiation oncologist and her nurse to discuss how I was doing, including the side effects of radiation. Side effects varied, from burning (like a bad sunburn) and swelling, to skin discoloration and fatigue. The fatigue surprised me. The therapy was so short; how could it be so tiring? The radiation oncologist explained it was cumulative; day after day of therapy added up and caused patients to tire. I’d be able to do my normal activities during radiation, she explained, but not much more than that. She was right. During radiation, I was wiped out and needed more downtime that I had anticipated. I also suspect that driving into the hospital every day for those four weeks contributed to my fatigue. It wasn’t easy to be reminded day in and out that I had cancer. The hospital, no matter how excellent the care, has a way of making you come face to face with your illness. At home, it’s easier to hide away from it.
The side effects of radiation therapy can last for weeks, even months afterward, so the best advice I have for anyone about to start radiation is to be kind to yourself. (In all truth, that’s my advice to everyone, everyday.) Be okay with declining invitations and taking more time for sleep and relaxation. Think about scheduling trips or visitors for after radiation concludes. Making choices that make you feel better, and stronger, will make the radiation process easier to handle.
Four months after finishing radiation, I had my follow-up appointment with my radiation oncologist during which she gave me the all clear. It was exactly what I wanted to hear, words everyone with a cancer diagnosis looks forward to receiving.
Those looking for more information may find these resources helpful in explaining the ins and outs of radiation therapy: Cancer.gov, Breastcancer.org, and American Cancer Society.

Continued Love, Thoughts and Prayers coming your way daily from me. Miss you, Love You, as always wish i was closer to help out but also to see you more on a regular basis. When we were younger the yearly visits were great and maybe we can start that again with us when life is back to a somewhat normal schedule for you. I really truly mean that. Again, Love you and take care, you are a brave, strong woman.
Great piece kid. Eight years later and I can’t find my dots to show off to my grandkids.????
Just reading this now. You are brave and strong and thoughtful. So happy this phase is over for you. I love you, friend.